PERIPHERAL ARTERY DISEASE OF THE LOWER EXTREMITIES
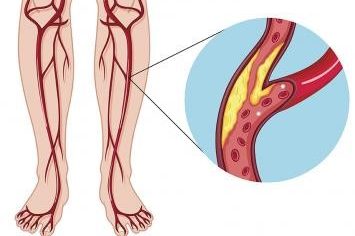
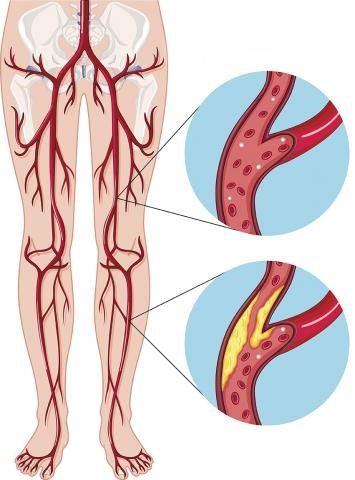
Peripheral artery disease (PAD) is a common disease of the lower limbs arteries. It is caused by the narrowing of the arteries, leading to the decrease in the flow of oxygenated blood to the tissues. Arteriosclerosis is considered as a common cause. Symptoms include numbness, reduced temperature in affected limb, and pain in the thighs, calves or feet. This disease possibly damages nerves, other tissues and organs in the affected limb.
REASON
The atheroslerotic plaques of the arterial wall, which is the formation of lipids, cholesterol, narrow the artery. Arterial walls become harder and cannot dilate, resulting in the muscles in the legs not receiving enough blood and oxygen while working hard, such as exercising or walking. This causes muscle pain.
Moreover, significant narrowing of the artery can cause muscle anemia even when the muscles are resting, leading to prolonged and constant pain.
RISK FACTORS:
This condition usually affects men over 50 years old, but women can also get it. People who have each of following factors might take a higher risk of suffering from PAD:
● Smoking
● Increase in Cholesterol levels
● Diabetes
● Cardiovascular diseases (coronary artery disease, hypertension, chronic kidney disease, cerebrovascular disease)
SYMPTOMS:
The common symptoms of peripheral artery disease of the lower extremities are:
- Pain, soreness, fatigue, in the muscles of the feet, calves or thighs.
- Burning sensation or discomfort in the affected limb.
These symptoms usually appear during walking or exercising, and disappear after a few minutes of resting.
At first, these symptoms may appear only when walking uphill, walking at high speed or hiking.
Then, these symptoms occur earlier, even when doing less exercise.
COMPLICATIONS:
If PAD is not treated, patients might face up with following complications:
● Ulcers, which is difficult to be treated.
● Pain and cramps at night
● Pain or itchy in the feet or toes, which can cause discomfort when clothes our bed sheet touch the skin
● Pain is worsen when you elevate your legs and relieved when you lower your legs and swing over the edge of the bed
● Disability of the lower limb
CLINICAL FEATURES:
During physical examination, the doctor can find:
● Arterial murmur during auscultation
● The blood pressure calculating at the ankle is lower than at the branchial
● Absent or diminished pulses at the ankle
If this disease become chronic, more symptoms might be detected, such as:
● Atrophied calf muscle
● Loss of hair on the legs, feet, and toes
● Ulcers, which is difficult to treat
● Skin discoloration or white nails on the toes
● Dry and thickening of the nail
Some tests can detect following symptoms:
● Calculate ankle-brachial index (ABI) less than 0.9
● Blood tests can cause high cholesterol or high blood sugar
● Doppler ultrasound of the lower extremities
● Angiogram of the lower extremities (with CT angioplasty – CTA or Vascular MRI – MRA)
LIFESTYLE MANAGEMENT CAN HELP PREVENT AND CONTROL THIS DISEASE:
- Do exercise:
- It is important to have advice from a specialist in order to have an appropriate exercise program. It is recommended that you should exercise for at least 30 minutes a day.
- Practice walking or elevating leg exercises ( cycling, swimming, climbing, etc.)
- Practice until muscle pain appears, then stop moving.
- After that, take a rest to relieve pain, then continue to exercise.
- Day by day, the circulation in the lower extremities may improve.
- Quit smoking:
- Give up smoking immediately
- Stay away from tobacco smoke ( passive smoking ).
- Because smoking can block the artery, reduces the blood’s ability to transfer oxygen and increases the risk of forming blood clots.
- Keep fit and stay healthy:
- Keep an appropriate weight ( BMI range 19-23 )
- Eating healthy foods, eating less and joining a weight loss program if you need to lose weight.
- Take care of your feet:
- Pay attention to your feet, especially if you have diabetes.
- Wear shoes that comfortably fit your feet, and can protect the tips of the toes.
- Pay attention to any cuts, scrapes, or wounds on your feet. You must go to the doctor immediately if the wound heals slowly or shows signs of infection.
- Manage other diseases:
- Control your blood sugar if you have diabetes.
- Manage stress through special psychological counseling, or participate in sports, meditation or yoga.
- Manage your blood cholesterol level by having a diet that is low in cholesterol and fat.
- Limit your alcohol intake: maximum 1 cup per day (women) and 2 cups per day (men).
- Control your blood pressure.
USING DRUGS:
These drugs can be used as assistance, but should be prescribed by your doctor:
- Aspirin or clopidogrel:
- Helps inhibit the aggregation of platelets in the blood in the arterial layer of arteries.
- DO NOT stop using this drug without being consulted by your doctor.
- Cilostazol:
- Helps dilate the arteries
- Cholesterol lowering drugs.
- Neuropathic pain relievers:
- Use if there is a presence of pain.
IS SURGICAL INTERVENTION NECESSARY?
Surgical interventions, surgery may be ordered by a vascular specialist in some following cases:
- Serious obstruction, causing acute ischemia or severe leg muscle pain leading to limited mobility.
- Malnutrition in the lower extremities, leading to ulcers which are difficult to heal.
SO, WHEN DO YOU NEED TO SEE THE DOCTOR FOR EARLY DETECTING THIS DISEASE?
See your doctor immediately if you have one of the following symptoms:
● Temperature of your feet skin decrease, discolored feet skin, numbness
● Chest pain or difficulty in breathing, with leg pain when walking or even while resting
● Red, hot, or swollen feet
● Having wounds and sores that are difficult to heal